Combatting Alzheimer's Disease Using Nanoparticles
Alzheimer’s Disease (AD) is the most common neurodegenerative disease in the world, characterized by progressive memory and cognitive dysfunction due to irreversible neuron degeneration. The disease is caused by aggregations of extracellular amyloid plaques in the brain, which are formed by interwoven β-amyloid fibrils. Since the plaques prevent neuronal signaling, AD eventually leads to total loss of autonomy and eventually to death.
Prevalence and Economic Impact
It currently affects nearly 30 million people worldwide, with a forecast of 60 million by 2050. There has been an 89% increase in deaths due to Alzheimer’s between 2000 and 2014. In America alone, the cost of Alzheimer’s also continues to rise, from $259 billion in 2017 to as much as $1.1 trillion by 2050, equivalent to a third of Medicare dollars spent.
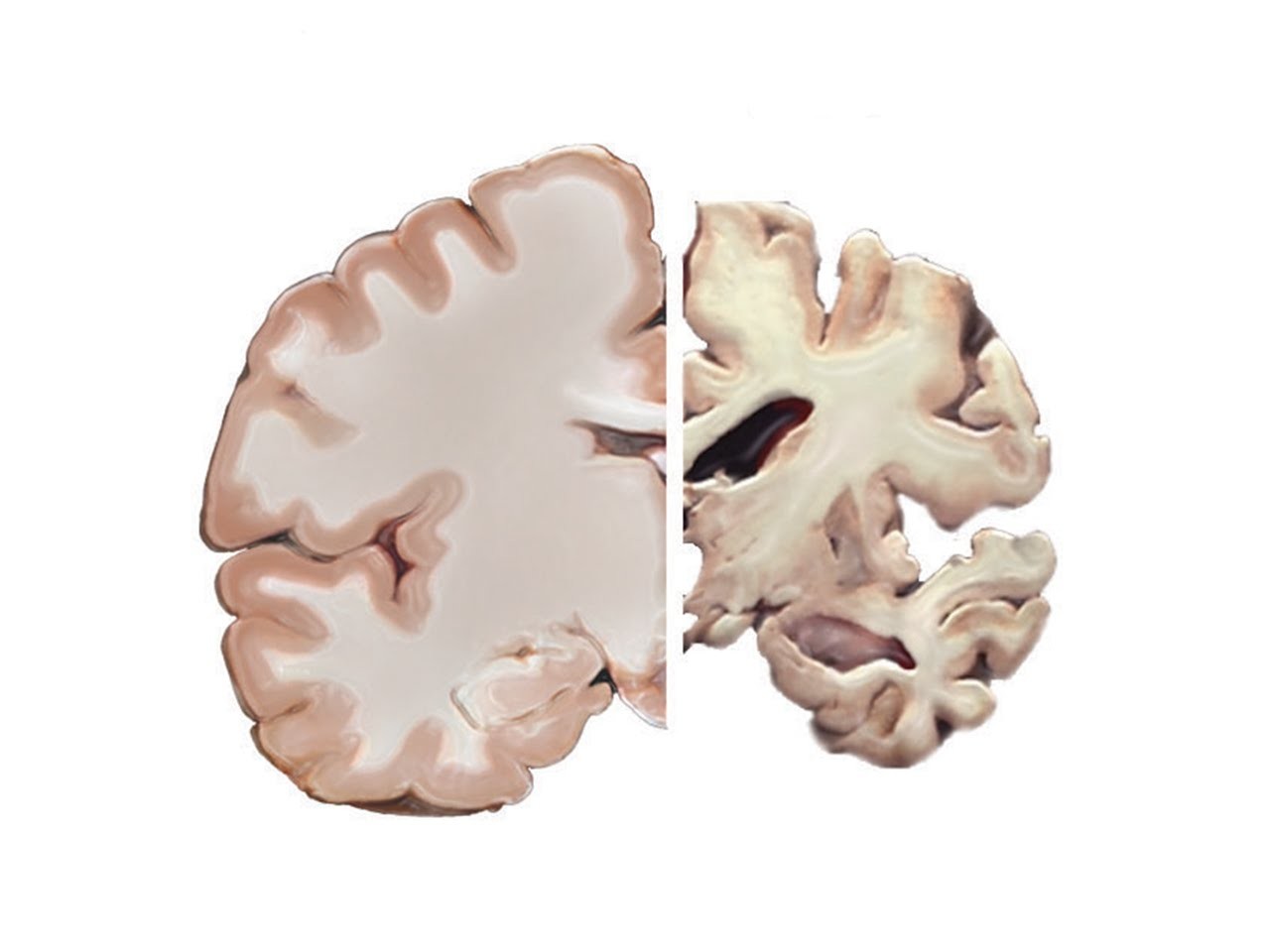
Figure 1. Comparison of Normal Brain to patient diagnosed with Alzheimer's Brain.
There has been an 89% increase in deaths due to Alzheimer’s between 2000 and 2014. There is no cure for Alzheimer’s Disease and current medication can only temporarily slow the worsening of symptoms, but only in the first stages of the disease. Established treatments provide only transitory symptomatic relief, temporarily improving cognitive function, but do not slow the long-term progression of the disorder; early detection is thus of crucial importance.
Nanoparticles as a Theoretical Treatment
However, there is a theoretical treatment in the making that may serve to improve treatment effectiveness: nanoparticles.
Nanoparticles are any particle less than 100 nanometers. Scientists have been developing unique nanoparticles that are meant specifically for drug delivery. These nanoparticles are so small that they can noninvasively penetrate most biological barriers, and may even hold the potential to cross the blood-brain barrier, which prevents foreign substances from entering and causing trauma to the brain. This would yield a more effective diagnosis and treatment for Alzheimer’s patients.
Superparamagnetic Iron Oxide Nanoparticles (SPIONs)
Several nanoparticles are currently being researched, however superparamagnetic iron oxide nanoparticles or SPIONs are considered the most promising nanotechnology for Alzheimer’s, capable of both diagnosing and treating the disease. The method is as follows:
- SPIONS are coated with silica molecules and Thioflavin-T (ThT), a non-toxic fluorescent dye that helps nanoparticles bind to amyloid beta plaques, important later in the method.
- These nanoparticles can then be immersed in a phosphate buffered saline solution and introduced into the body through femoral intravenous injection. Once injected, the nanoparticles are incubated for a period of 30 minutes.
- Following the incubation, the magnetic properties and fluorescent dye of the nanoparticles cause them to bind to aggregates of amyloid plaques in the brain.
- Due to the metallic properties of nanoparticles, they are visible as small circular areas in MRI scans.
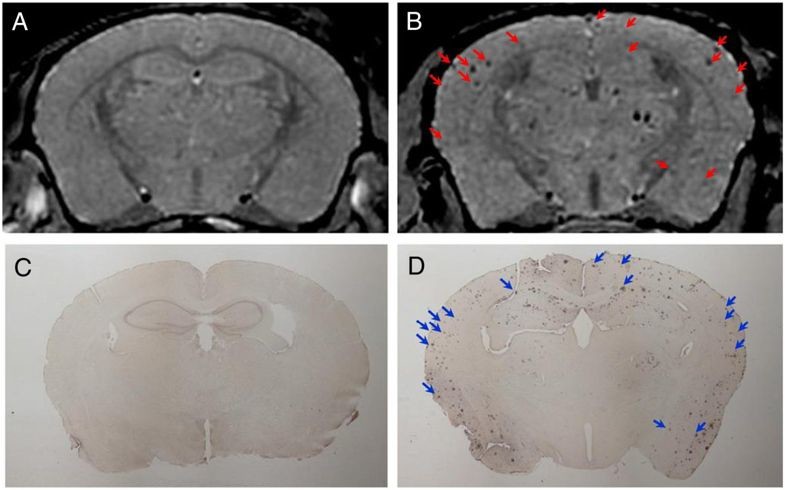
Figure 2. The inducible magnetization of magnetite particles allows them to be directed to a defined location in the presence of an externally applied AC field.
Diagnostic and Therapeutic Potential
This technology would allow doctors to diagnose Alzheimer’s disease beyond doubt for the first time, because currently doctors cannot confidently diagnose Alzheimer’s until later stages of the disease, and cannot absolutely diagnose the disease until after the patient's death. Thus, this method offers the first absolute diagnostic for patients.
This technology would allow Alzheimer’s to be diagnosed at an earlier stage because the aggregates are easily visible, allowing better treatment of the disease and better overall outcomes for patients.
In addition to diagnostic ability, SPIONs also have the potential to inhibit amyloid beta-peptide formation because when an alternating current is applied to the brain, the magnetic properties of the nanoparticles cause the amyloid beta fibrils to separate, preventing the accumulation of amyloid plaques, thus lessening the effect of Alzheimer’s disease.
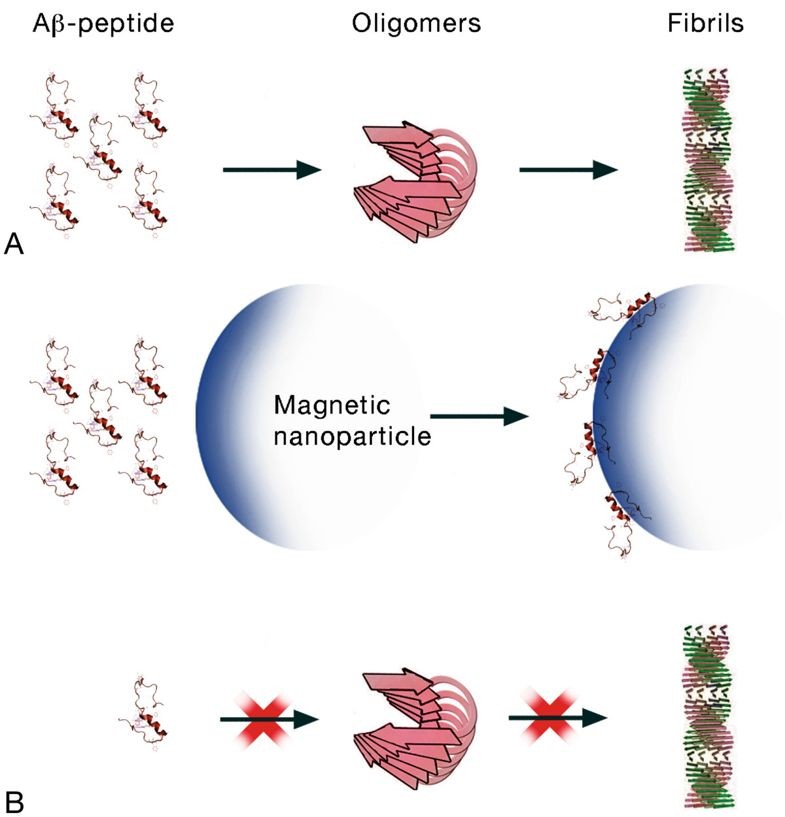
Figure 3. (A) the usual sequence when the Aβ-peptides turn into fibrils and (B) the potential sequence when Aβ-peptide monomers are attached to the surface of the SPIONs decreasing the free Aβ-peptide concentration, lowering the chance of forming oligomers and fibril.
Conclusion
Due to their high biocompatibility and superparamagnetic properties, SPIONS are valuable in treating and diagnosing Alzheimer’s. This is because they are capable of acting as a magnetic contrast agent and fluorescent dye for detection and also as an inhibitor for the aggregation of amyloid fibrils. SPIONs have far-reaching applications beyond Alzheimer’s disease, in biotechnology, drug delivery, and imaging. However, their novelty means that side effects are unknown and further testing and development is needed to help patients with this technology.
What is ultimately so amazing about SPIONs is that they are able to tackle the direct cause of Alzheimer’s unlike any method currently used. The use of these new therapeutic tools is bound to unleash a new era of possibility for patients currently suffering from extremely debilitating diseases without effective forms of treatment. It is clear that nanomedicine will lead the charge to that new reality.
© Will Blair.RSS