Personalized Medicine in the Treatment of Cystic Fibrosis
Over the summer, I had the tremendous privilege of attending the Yale Young Global Scholars program at Yale University. The program, to me, was a truly incredible experience to explore a wide range of topics in biology and medicine and meet amazing people from around the world. As a component of the program, we were tasked to explore a concept in biology and present our findings to our fellow students and Yale instructors and faculty. I, along with 4 other students, decided to investigate personalized medicine, a topic which had drawn our attention at a lecture the previous day. Within personalized medicine, we focused on cystic fibrosis, asking the question “should personalized medicine be used to treat cystic fibrosis.” Cystic fibrosis is the most common fatal genetic disease in the world, with 70,000 affected people, each with an average life expectancy of 37 years.
Understanding Cystic Fibrosis
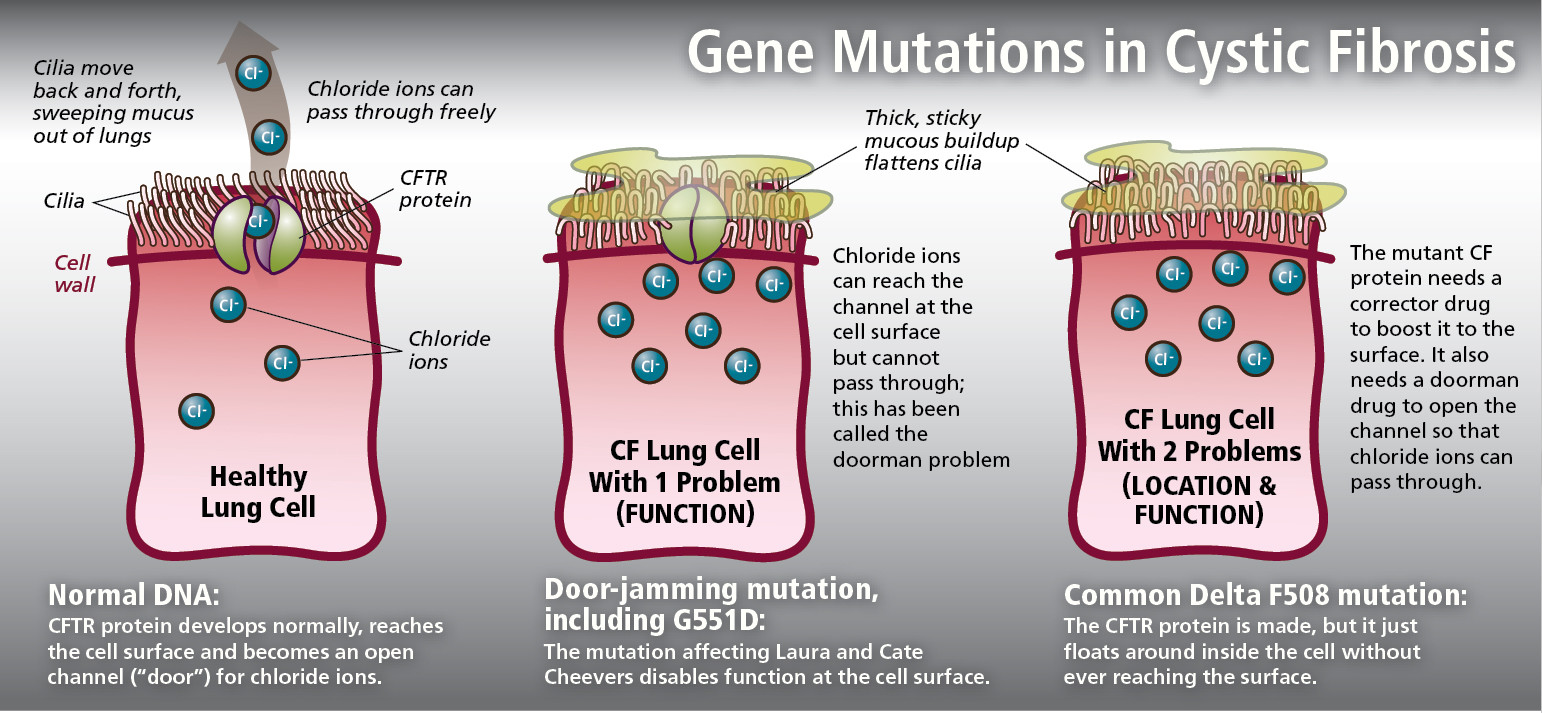
Cystic Fibrosis results from a mutation in the Cystic Fibrosis Transmembrane Regulator (CFTR) gene. The CFTR gene acts as a channel for the movement of chloride ions in and out of cells, which in turn helps to regulate the movement of water in and out of the cells due to differences in concentration gradients. As a result, mutations in the CFTR gene, of which there are more than 2000, lead to the buildup of mucus in the lungs and restricted ability to breathe, as well as inflammation, severe lung damage, and pancreatic deficiency.
What is Personalized Medicine?
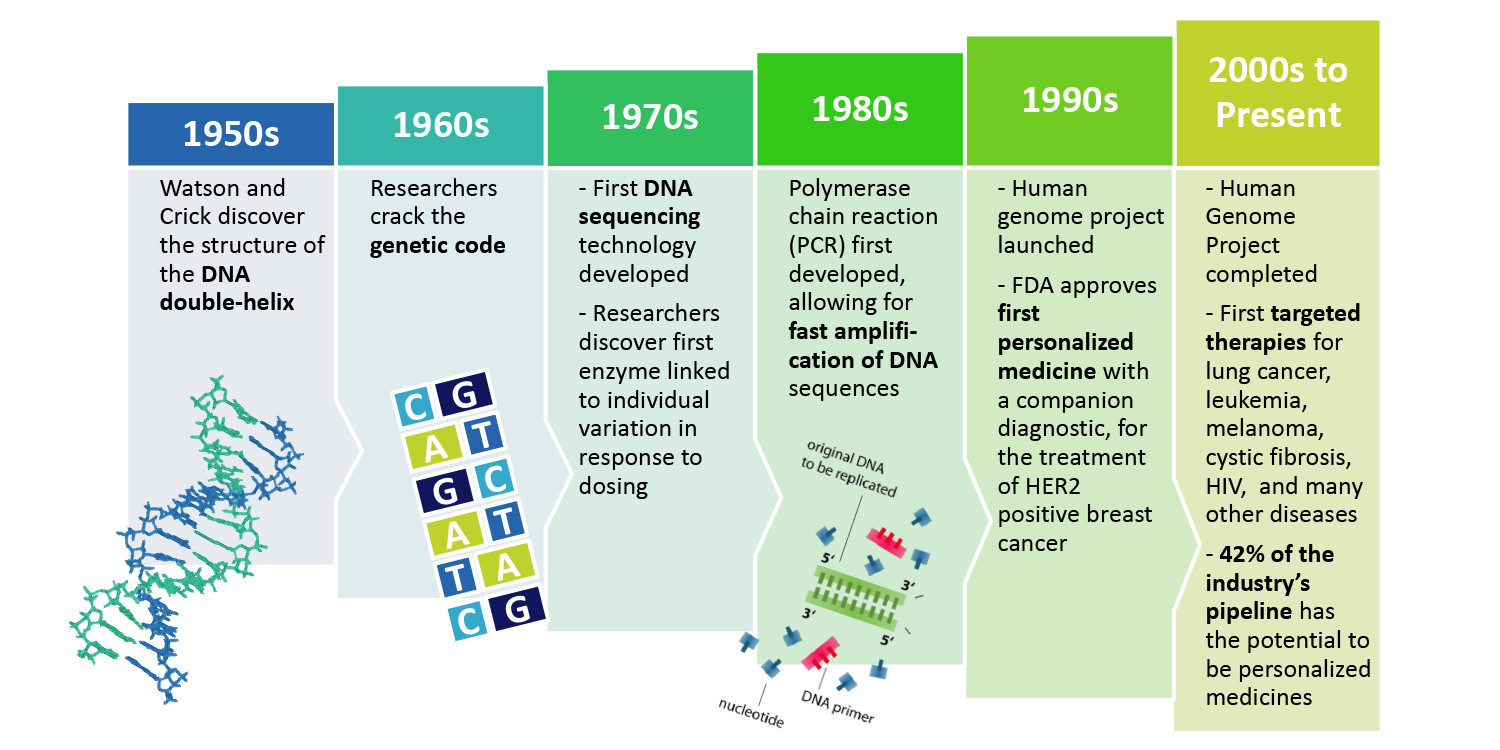
This is where personalized medicine comes into the equation. Personalized medicine is defined by the National Human Genome Research Institute as the “use of an individual’s genetic profile to guide decisions made in regard to the prevention, diagnosis, and treatment of disease.” Personalized medicine tailors an individualized approach for every patient using diagnostic testing. As opposed to one-size-fits-all medicine, which has been, and is currently, the status quo, personalized medicine tailors an individualized approach for every patient using diagnostic testing. Personalized medicine was created in the early 1990s when a company called Roche noticed that one drug can produce different responses in different individuals.
Current Treatments for Cystic Fibrosis
The current forms of treatment for cystic fibrosis include airway clearing techniques (ACTs), which may consist of coughing or chest physical therapy, to loosen thick and sticky mucus. Medications are also prescribed to help keep lungs clear and prevent infections. Lastly, lung transplants are also common, and ostensibly drastic, treatment of cystic fibrosis to extend and improve the quality of life of patients with severe lung damage. Although these methods have the ability to alleviate symptoms of cystic fibrosis, new drugs based on each individual person’s DNA are far more effective.
New Drugs for Cystic Fibrosis
New drugs have been created to treat cystic fibrosis in a new and innovative way, by targeting the mutation that causes cystic fibrosis. There are two major personalized medicines which have emerged in recent years to treat cystic fibrosis. These are Orkambi and Kalydeco. Orkambi has the ability to treat approximately 70% of cystic fibrosis cases, and Ivacaftor has the capability to treat 7% of cases. Orkambi is a drug combination aimed at repairing the Delta-F508 mutation. Delta F508, found in 70% of patients, prevents the CFTR protein from being properly constructed during DNA transcription. Despite some success of the drug in treating cystic fibrosis, recent studies done with Orkambi have suggested that it increases patient’s lung function and BMI. Furthermore, it reduced pulmonary exacerbations and other adverse respiratory symptoms. Possible side effects included the development of cataracts in children and respiratory discomfort. Kalydeco (Ivacaftor), alternatively, has been much more successful in its treatment of cystic fibrosis patients with the G551D mutation, which it targets. The G551D mutation prevents the chloride funnel formed by CFTR proteins from opening and closing. Ivacaftor, instead, helps to keep these channels open, mitigating the buildup of mucus. Ivacaftor is truly a breakthrough therapeutic agent and several studies have shown the benefits of the drug including reporting less coughing, mucus, and trouble breathing. The drug also caused an average weight gain of 6 pounds, an incredible effect as many cystic fibrosis patients have great difficulty in gaining any weight. While Ivacaftor has shown these numerous positive effects it does only target a single mutation of the 2000 total. However, the G551D and Delta-F508 mutation both account for an overwhelming majority (77%) of CFTR mutations, allowing these drugs to treat most cystic fibrosis patients.
Future Directions
What’s Next
Other drugs are being developed in order to target other variations of CFTR mutations. In addition to Ivacaftor, a new drug called Ataluren is on the horizon. Ataluren is an oral drug that is currently being developed by PTC Therapeutics, a company in the Netherlands, attempting to find alternative ways to treat the Delta-F508 Mutation. In 2016, the cystic fibrosis foundation opened a new lab in Lexington, Massachusetts. This lab is dedicated to researching the causes of cystic fibrosis and how it can be treated. Researchers are beginning to research stem cells and explore gene editing to better treat cystic fibrosis.
Should Personalized Medicine be Used to Treat Cystic Fibrosis?
Our group came to the unanimous conclusion that personalized medicine is an extremely important innovation in medicine, and it would be greatly beneficial to patients with a wide variety of diseases, including cystic fibrosis. There are three reasons why personalized medicine is so much better than current methods used for treatment of cystic fibrosis, and the vast majority of diseases:
- Personalized medicine treats the underlying cause of the disease: Current methods of cystic fibrosis treat only the symptoms of the disease whereas personalized medicine treats its underlying cause. Better matching of patients to drugs instead of “trial and error.”
- The benefits of the drug outweigh the side effects: Although there are some side effects to both Orkambi and Ivacaftor, these are not severe enough to warrant the drugs’ disuse. In addition, personalized medicine may eliminate life-threatening adverse reactions of current drugs.
- Personalized medicine offers a future of discovery and advancement: As personalized medicine continues to evolve and advance, more drugs will be developed that target other mutations of cystic fibrosis. In other words, this is just the beginning.
Conclusion
Clearly, personalized medicine is an extremely important avenue of medicine which will undoubtedly form the future of healthcare. However, as we continue to develop personalized medicine, there are a few ideas we can keep in mind to make it better.
- Improve the cost/affordability of these drugs: Drugs must be made accessible to all patients if personalized medicine is to become the future of medicine. For instance, Kalydeco costs more than 300,000 dollars per year for use.
- Improve drugs to ameliorate adverse side effects: The adverse side effects of many of these drugs must be limited to ensure that they do not inhibit the quality of the treatment or patient health.
- Gain greater understanding of drugs: Many drugs are developed through a process called high throughput screening whereby thousands of drug-like molecules are randomly applied to mutated cells until a combination works. This leaves a critical knowledge gap: we know that these drugs work, but we do not know how they work.
The advent and revolutionary power of personalized medicine will dramatically improve healthcare by providing accurate diagnosis and treatment to ensure that patients receive drugs that correspond to their unique individuality. Personalized medicine has the ability to treat a wide range of diseases with accuracy and precision, and will beckon a new age of unlimited discovery in medicine and healthcare. Questions remain about the capacity of personalized medicine, however, it is clear that we have only reached the frontier of personalized medicine, and there is so much more to discover.
© Will Blair.RSS